Meningitis - Classification, Purulent, Aseptic, Tuberculous, Chronic, Acute, Pathogenesis
Classification of meningitis
Classification of meningitis can be done on the basis of:
By Clinical agenda
It is based on the host's response to invading microorganisms. It can be categorized into:
Purulent meningitis
Aseptic meningitis
Tuberculous meningitis
Purulent meningitis
In Purulent meningitis, the patient has a marked, acute inflammatory exudative CSF containing a large number of polymorphonuclear cells (PMNs) i.e. 100 to several thousand leucocytes/mm3.
Aseptic meningitis
Aseptic meningitis is the inflammation of the meninges in patients whose cerebral spinal fluid test result is negative with routine bacterial and fungal cultures. It may be caused by bacteria, viruses (the most common causative agent), fungi, or cancer malignancies.
The condition is characterized by an increase in lymphocytes and other mononuclear cells (pleocytosis) in the central spinal fluid (CSF) i.e. 10-50 cells/mm3. It is usually self-limiting with symptoms such as fever, headache, stiff neck, nausea, and vomiting.
CSF is mostly clear/slightly turbid but during aseptic meningitis, the glucose level in CSF remains normal, and the protein CSF level may be slightly elevated.
The condition can also be a symptom of syphilis, and spirochete disease (i.e. leptospirosis and Lyme borreliosis) while stiff neck and pleocytosis are also associated with malignancy.
Tuberculous meningitis
Tuberculous meningitis is a form of meningitis caused by Mycobacterium tuberculosis. It is one of the severe complications of tuberculosis which may manifest as intermittent or persistent headaches. Tuberculous meningitis is usually fatal if prompt treatment is not started and may have been a result of primary pulmonary tuberculosis.
In such cases, fibric clot develops in CSF if left undisturbed.
*Fibric clot = Veil clot = unique symptom of meningitis caused by M. tuberculosis.
By duration
Acute meningitis (symptoms develop within a few days)
Subacute meningitis (symptoms develop over days to a few weeks)
Acute meningitis
Symptoms of acute meningitis include fever, stiff neck, headache, nausea, vomiting, neurologic abnormalities, change in mental status, and seizures (20-30%). The highest incidence of acute meningitis in neonates (20% mortality).
In individuals with acute meningitis,
the CSF contains a large number of inflammatory cells ( >1000/mm3), primarily PMNs
CSF has decreased glucose level relative to serum glucose level
increase in CSF protein concentration
Acute sequelae include cerebral edema, hydrocephalus, cerebral herniation, and focal neurologic changes. Permanent deafness occurs in 10% of children who recover.
Chronic meningitis
Chronic meningitis usually occurs in immunocompromised individuals but this is not always the case. An abnormal number of White Blood Cells (WBC), elevated protein, and a decrease in glucose level can occur in CSF.
Symptoms include fever, headache, stiff neck, nausea, vomiting, lethargy, confusion, and mental deterioration. The symptoms may persist for a month or longer before treatment is initiated.
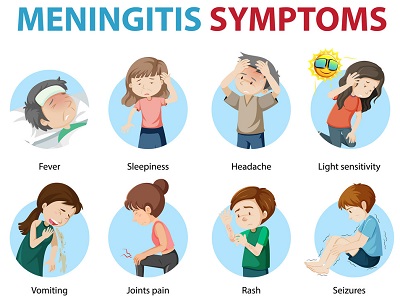
Fig: Meningitis (Source: VectorStock)
Pathogenesis of Meningitis
The respiratory tract is the primary portal of entry for many etiologic agents of meningitis. Most cases of meningitis are a result of bacteremia.
The successful meningeal pathogen must first colonize and cross host mucosal epithelium, then enter and thrive within the bloodstream by evading host defenses at each level.
Eg: S. pneumoniae and N. meningitis secrete IgA protease that destroys host secretory IgA. They are capsulated, thus preventing phagocytosis.
Microorganisms enter Central Nervous System (CNS) by interacting and subsequently breaking down the Blood-brain barrier's (BBB) microvascular endothelium. Adhesion is facilitated by pilli, capsule, and lipoteichoic acids of the microorganism.
Organisms can then enter the brain
through loss of capillary integrity by disrupting the tight junction of BBB
through transport within circulating phagocytes
by crossing endothelial cell lining within endothelial cell vacuoles
After gaining access to the host brain, they multiply within the central spinal fluid (CSF).