Naegleria fowleri - Clinical manifestation, Prognosis, Laboratory diagnosis
Clinical manifestation of Naegleria fowleri
Naegleria fowleri is the causative agent of primary amoebic meningoencephalitis (PAM), severe hemorrhagic meningoencephalitis.
Primary Amoebic Meningoencephalitis (PAM)
this condition is mainly seen in children and young adults who were previously healthy
the patients have a history of bathing, swimming, diving, or playing in warm, stagnant, or freshwater
the incubation period of Naegleria fowleri may be short, 2 days to 3 days but sometimes may be as long as 7 to 15 days
clinical symptoms of PAM, which is acute and fulminant, mimic that of acute bacterial meningitis which is abrupt on onset and brief in duration
initial symptoms include sudden onset of severe, persistent bifrontal or bitemporal headache which is followed by fever (38.2°C to 40°C), nausea, projectile vomiting, mental status change, stiff neck, seizures, abnormalities in taste (ageusia), abnormalities in smell (parosmia)
as the infection progresses, drowsiness, convulsions, photophobia, and coma are observed
Prognosis of Naegleria fowleri
the prognosis of PAM, caused by Naegleria fowleri, is very poor and in most cases is fatal with above 95% mortality
death occurs due to cardio-respiratory arrest or pulmonary edema within a week of the appearance of the initial symptoms
Laboratory Diagnosis of Naegleria fowleri
Naegleria fowleri is diagnosed in the laboratory by the following procedure:
Specimen
For lab diagnosis of Naegleria fowleri, samples usually collected include:
CSF
biopsy brain tissue
Microscopy
The diagnosis of Naegleria fowleri depends upon the detection and identification of the trophozoite form under a microscope.
CSF is centrifuged at 150xg for five minutes, the supernatant is aspirated and the sediment is suspended in the remaining fluid. A drop of sediment suspension is observed under a microscope at 10x and 40x magnification.
Naegleria fowleri is detected by their active directional movement but the trophozoites should not be confused with leucocytes. Direct fluorescent antibody staining method or other stains such as trichrome, Giemsa, and Wright stains can be used in CSF smears for identification
In histologic brain biopsy tissues, trophozoites can be identified by using immunofluorescence and immunoperoxidase methods
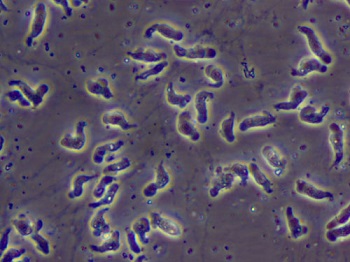
Image: electron microscopy of N. fowleri (Source: CDC)
Culture
Infection by Naegleria fowleri can be confirmed by culture of the specimen on non-nutrient agar plates incubated with Gram-negative bacteria such as E. coli. In positive cases, trails are left by migrating amoebae where the lawn of bacteria is observed.
Serodiagnosis
Since the Naegleria fowleri infection is rapid and the parasite does not initiate the host immune response, serodiagnosis methods are not useful in diagnosis.
Molecular diagnosis
Molecular diagnosis is done mostly for research purposes:
DNA probes
PCR
Imaging methods
CT scan
Although a CT scan of the head is not diagnostic, it does show the loss of the subarachnoid portion and shows diffuse gray matter enhancement which is a characteristic of Naegleria fowleri.
Other tests
Since the CSF level is elevated and is hemorrhagic, the CSF specimen is bloody and shows a strong neutrophilic reaction
The protein content in the CSF during Naegleria fowleri is elevated while the glucose level of the CSF is normal or low
CSF shows a pleocytosis with increased WBC and RBC counts.