Toxoplasma gondii - Clinical manifestation, Complications, Prognosis
Clinical manifestation of Toxoplasma gondii
Toxoplasmosis, caused by Toxoplasma gondii, may clinically manifest as acquired, congenital, ocular infections in immunocompetent hosts while in an immunocompromised host, the manifestations are more severe.
Congenital toxoplasmosis
congenital toxoplasmosis occurs when a non-immune susceptible woman is infected during pregnancy
Toxoplasma gondii is transmitted through the placenta to the fetus
the disease is much more severe if the infection is acquired during the first trimester of pregnancy
may lead to stillborn or miscarriage
congenital toxoplasmosis occurs in 17% of cases
if the infection occurs during the last trimester of pregnancy, the infant at the time of birth may show mild to no symptoms
about 65% of cases occur during the last trimester of pregnancy
cerebral calcifications, convulsions, and retinochoroiditis occur with congenital toxoplasmosis- retinochoroiditis being the most common (75%-80% of cases)
other less frequent manifestations include microcephaly, hydrocephalus, mental retardation, anemia, jaundice, thrombocytopaenia, and organomegaly
chronic infection does not lead to congenital toxoplasmosis i.e. if a mother had toxoplasmosis prior to the current pregnancy, the transplacental transmission does not occur
around 80%-90% of pregnant women with toxoplasmosis are clinically asymptomatic while 10%-20% of pregnant women with toxoplasmosis show clinical symptoms- most commonly lymphadenopathy
Acquired toxoplasmosis
Although toxoplasmosis is a benign and self-limiting condition in an immunocompetent host, acquired toxoplasmosis is serious and life-threatening in immunocompromised individuals. They are classified into
toxoplasmosis in immunocompetent individuals
toxoplasmosis in the non-AIDS immunocompromised host
toxoplasmosis in AIDS patients
Toxoplasmosis in immunocompetent individuals
Benin and self-limiting Toxoplasma gondii infection
acute toxoplasmosis is asymptomatic in 80% to 90% of cases while 10%to 20% are symptomatic
the most common clinical symptom is lymphadenopathy in which deep cervical lymph nodes are affected
uncommon sites infected by Toxoplasma gondii include supraclavicular, suboccipital, axillary, and inguinal lymph nodes
the infected lymph nodes are characterized by discrete, non-tender, with varying firmness
other symptoms include fever, sore throat, myalgias, night sweats, malaise, maculopapular skin rash (does not affect palms or soles), and retinochoroiditis (10% of cases)
in rare cases, abdominal pain with retroperitoneal and mesenteric lymphadenopathy is seen
Toxoplasmosis in the non-AIDS immunocompromised host
Toxoplasma gondii infection is seen in immunosuppressed individuals undergoing immunosuppressive therapy for malignancies (Hodgkin disease, leukemia) or patients who have under bone marrow transplant or solid organ transplantation
the toxoplasmosis may be newly acquired or chronic (due to reactivation)
the central nervous system is affected in 50% of cases
common symptoms include hemiparesis, seizures, change in visual and mental status
other severe clinical manifestations are encephalitis, meningoencephalitis, space-occupying lesions
non-neurological symptoms include myocarditis and pneumonitis
Toxoplasmosis in AIDS patients
Toxoplasma gondii infections in AIDS patients are the most severe and often fatal
the brain is commonly infected in the majority of cases with the characteristic feature being Toxoplasmic encephalitis (TE) with or without focal CNS lesion
common symptoms include seizures, meningismus, neuropsychiatric, altered mental state, sensory abnormalities cerebellar signs
although the lung is not usually infected, pulmonary toxoplasmosis is now being increasingly recognized in patients with AIDS without proper therapeutic and clinical management
pulmonary toxoplasmosis mostly occurs in AIDS patients whose CD4 count is less than 50 cells/mm3 and manifests as febrile illness, dyspnoea, and cough
extra-pulmonary manifestation is seen in 50% of cases
the less common syndrome is toxoplasmic chorioretinitis
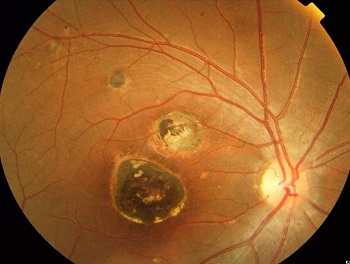
Image: Macular retinochoroidal lesion of congenital ocular toxoplasmosis (Source: eophtha)
Ocular toxoplasmosis
the hallmark of ocular toxoplasmosis is focal necrotizing retinochoroiditis
this manifestation accounts for about 35% of chorioretinitis in both children and adult
ocular toxoplasmosis mainly occurs due to congenital infection
in acquired infection chorioretinitis is unilateral while in bilateral infection, chorioretinitis is bilateral
symptoms are blurred vision, photophobia, pain, and scotoma
Complications of Toxoplasma gondii
Congenital toxoplasmosis complications include symptoms such as seizures, deafness, and mental retardation.
The complication of ocular toxoplasmosis, caused by Toxoplasma gondii, is partial or complete blindness.
Central nervous system toxoplasmosis may become complicated with a seizure disorder or focal neurologic deficits
Prognosis of Toxoplasma gondii
The prognosis of Toxoplasma gondii is good in an immunocompetent host.
In immunocompromised individuals, the host prognosis is poor due to relapse if treatment is stopped.
In cases of HIV patients infected with Toxoplasma gondii, the mortality is high i.e. at 35%.