Entamoeba histolytica - Laboratory Diagnosis
Laboratory Diagnosis of Entamoeba histolytica
The process of laboratory diagnosis of Entamoeba histolytica is done by the following the process depending upon intestinal amoebiasis, or Amoebic liver Abscess (ALA).
For Intestinal amoebiasis
Sample
The lab diagnosis of Entamoeba histolytica infection begins with the collection of samples:
stool (most common)
rectal exudates (collected by endoscopy)
rectal ulcer tissue (collected by endoscopy)
Microscopy
based on the detection of both Entamoeba histolytica trophozoites and cysts
specimens should be examined within 1-2 hours of defecation to demonstrate trophozoites
cysts can be observed in 3-day-old stool specimen
in case of delay, the specimen can be preserved in polyvinyl alcohol or refrigerated
for rectal exudates and rectal ulcer tissue, the trophozoites are seen in exudates covering rectal mucosa while in ulcer tissue where necrosis is present, trophozoites are less frequently observed
can be done by following methods:
* Direct wet mount microscopy
* Examination after concentration of stool
* Examination after staining
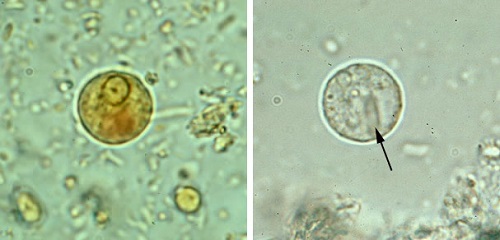
Image: wet mount microscopy of Entamoeba histolytica cyst with iodine stain (left), unstained (right) (Source: CDC)
Direct wet mount microscopy
the presence of mature Entamoeba histolytica quadrinucleate cysts or hematophagous trophozoites in stool confirms the infection
useful mostly in the detection of freshly passed diarrhoeic stool
the wet mount is prepared by mixing saline, iodine, or lactophenol cotton blue (LPCB)
saline water mount is useful for the detection of hematophagous trophozoites while iodine and LPCB are useful to stain cysts of Entamoeba histolytica as well as differentiate it from other protozoa or helminthic ova
a single sample observation has about 30-50% sensitivity while three consecutive stool specimen observations can increase the sensitivity to about 90%
Examination after concentration of stool
the formalin-ether method is used for the detection of cysts but trophozoites cannot be detected by this method
useful when the number of amoebae in the stool is scanty/in the case of chronic amoebiasis
Examination after staining
permanent stains such as iron-haematoxylin, trichrome, or periodic Acid-Schiff (PAS) are used to stain the stool sample before microscopic observation
PAS strains are more helpful in distinguishing internal structures of the trophozoites while trichrome stains best demonstrate intra-cellular structures of both trophozoites and cysts
Stool Antigen Detection
Counter-Current Immunoelectrophoresis (CIEP) and (Enzyme-Linked ImmunoSorbent Assay) ELISA are used in the detection of amoebic copro-antigen in stool samples
in ELISA, monoclonal antibodies for galactose (Gal)/N-acetyl-D-galactosamine (GalNAc) 170kD lectin present in pathogenic strains of Entamoeba histolytica are used to detect the specific protein
has a sensitivity of 100% and specificity of 97%
differentiates between Entamoeba histolytica and E. dispar
Stool Culture
Entamoeba histolytica can be cultured and isolated in Robinson’s medium and NIH polyxenic culture medium
has a sensitivity of 75%
used in asymptomatic cases, and chronic cases, and to harvest the parasite to determine the zymoderme patterns
Serodiagnosis
Antibodies specific to Entamoeba histolytica are produced in the host serum which can be detected by Indirect Haemagglutination (IHA), indirect fluorescent antibody (IFA), ELISA
used mostly in invasive intestinal amoebiasis but its sensitivity is at 50%
cant be detected in asymptomatic cyst passers
Molecular diagnosis
DNA probe = rapid and specific method
PCR = sensitivity at 87%, also differentiates between Entamoeba histolytica and E. dispar
For Amoebic liver Abscess (ALA)
Sample
The lab diagnosis of Entamoeba histolytica includes the following sample:
liver pus aspirates
Microscopy
in necrotic material collected from the center of the liver abscess, trophozoites are scanty while the trophozoites are abundant on the walls of the abscess
hence the last part of the liver pus aspirate is best for detection of the parasite under microscopy, culture in Robinson’s medium or NIH polyxenic culture medium, and antigen detection (Direct fluorescent antibody test)
Low sensitivity = 15%

Image: E. histolytica with visible consumed erythrocytes under a microscope (Source: Wikipedia)
Serodiagnosis
Serodiagnosis cannot differentiate between past and recent infections as high antibody titers may be present for years even after successful treatment
Detection of antibodies
IHA, rapid- IHA, protein A- IHA, IFA, and ELISA used to detect antibodies specifically in the serum
IHA
if IHA shows 1:128 amoebic antibody titer, an amoebic liver abscess may be present (crude plate – III D)
Polyxenic or axenically cultures are used as antigens
in cases, with ALA the sensitivity of IHA is 75-90%
in intestinal amoebiasis, the sensitivity of IHA is 50-60%
in asymptomatic cases, the sensitivity of IHA is 10%
ELISA
most extensively used method of diagnosis
IgG ELISA has sensitivity = 99% and specificity of more than 90% in ALA cases
Recently, genetically engineered polypeptides and purified recombinant amoebic antigens such as LC3 (recombinant cysteine-rich lectin-derived protein) have been used in ELISA which increases the specificity of the test
Simple Assay
Dot-ELISA
Staphylococci adherence test (SAT)
Carbon Immunoassay (CIA)
Molecular Diagnosis
PCR
Imaging methods
thoracic X-ray: shows right-sided pleural effusion masking right costophrenic angle and elevated right hemidiaphragm
Ultrasound: most commonly used
sensitivity = 70-80%
ALA appears as a homogenous hypoechoic round lesion
CT scan: 88-95% sensitiivty
in contrast CT-scan, ALA appears round, low-attenuation lesion with smooth margins and a contrast-enhancing peripheral rim
MRI
similar to ultrasound